Services
OFFICE SERVICES

Echocardiography
Echocardiography is a safe technique for taking pictures of the heart, including its valves, major veins, aorta, and chambers. It uses high-frequency ultrasound directed at the chest from various angles. Reflected sound waves create a two-dimensional heart image, showing blood flow through the chambers. This method detects subtle abnormalities missed during physical exams. It is particularly effective for analyzing heart murmurs and evaluating cardiac pump function. The procedure typically takes 15 to 20 minutes.

Ultrasound and doppler tests (carotid ultrasound, abdominal ultrasound, Venous duplex, Arterial duplex)
Using ultrasound, we can capture images of the carotid arteries, abdominal aorta, and peripheral vessels. This method accurately screens for conditions like carotid artery disease, peripheral artery disease, venous insufficiency, deep vein thrombosis, and abdominal aneurysms.

Treadmill Stress Testing
Walking on a treadmill helps us assess fitness levels and identify chest pain linked to cardiac ischemia. A technician, physician assistant, or doctor supervises the test, ensuring safety. The exercise proceeds in 3-minute stages until the person reaches a target heart rate or an endpoint. Despite decades of use, treadmill stress testing is only about 65% accurate in diagnosing coronary artery disease as a cause of chest pain.

Treadmill Stress Echocardiogram
This diagnostic test evaluates heart function and detects coronary artery disease. While exercising on a treadmill, the patient’s heart is monitored using an echocardiogram, which captures real-time images. Doctors assess blood flow and look for areas affected by blockages or other issues. The non-invasive test helps diagnose angina, heart attacks, or abnormal rhythms. It also evaluates the heart’s response to physical activity and the effectiveness of prior treatments.

SPECT myocardial perfusion imaging
Some people cannot perform treadmill tests due to arthritis, back pain, or abnormal ECGs. For these patients, we use nuclear imaging to evaluate the heart before and after administering medications like regadenoson, which briefly dilates coronary arteries.

PET myocardial perfusion imaging
Although better than treadmill tests, SPECT imaging has drawbacks, including a lengthy process (2–3 hours) and challenges interpreting images in obese individuals or those with significant soft tissue. PET imaging offers an alternative for these limitations.
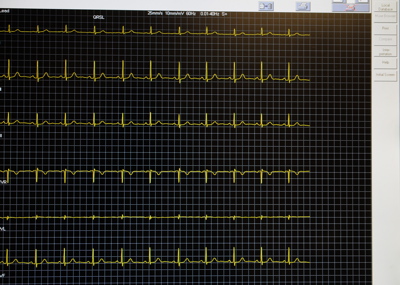
Cardiac monitor and long-term arrhythmia surveillance techniques
Palpitations or irregular heart rhythms can be intermittent, making them difficult to catch on a standard ECG. Holter monitors, which record heart activity for up to 48 hours or longer, help capture these events. Advanced patches are also available for up to 7 days. A cardiologist interprets the computer-analyzed recordings.

EECP (Enhanced External Counter Pulsation)
We use EECP to treat patients with angina that does not respond to traditional methods, such as bypass surgery, stents, or medications.

Pacemaker and AICD monitoring/programming
Our team provides care for patients with pacemakers or implanted cardioverter-defibrillators (AICDs). These devices help manage heart rhythm disorders like bradycardia or severe arrhythmias. We offer regular monitoring and programming to ensure optimal function tailored to each patient’s needs.

Tilt table testing
Tilt table testing helps diagnose fainting or lightheadedness by examining the body’s response to positional changes. This test provides insights into symptoms, guiding personalized treatments to prevent future episodes.

Leqvio infusion
Leqvio (inclisiran) is a new cholesterol-lowering medication that reduces LDL cholesterol by about 50%. Administered as a subcutaneous injection every six months, it offers a convenient alternative to daily or monthly treatments.

Rare Cardiac conditions treatment
We provide specialized care for rare conditions like TTR amyloidosis and hypertrophic obstructive cardiomyopathy (HOCM). These diseases require early detection and accurate diagnosis. Our team uses advanced tools and collaborates to create tailored treatment plans.
HOSPITAL SERVICES

Consultation and acute coronary care
Our board-certified cardiologists specialize in treating a wide range of heart conditions. Their extensive training ensures the delivery of advanced, effective care.

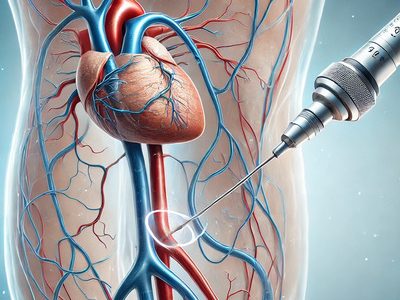
Diagnostic cardiac catheterization
Cardiac catheterization is the gold standard for diagnosing coronary artery disease and other heart conditions. It involves inserting a catheter into a blood vessel and guiding it to the heart. Using X-ray imaging and contrast dye, doctors evaluate blood flow and identify blockages.
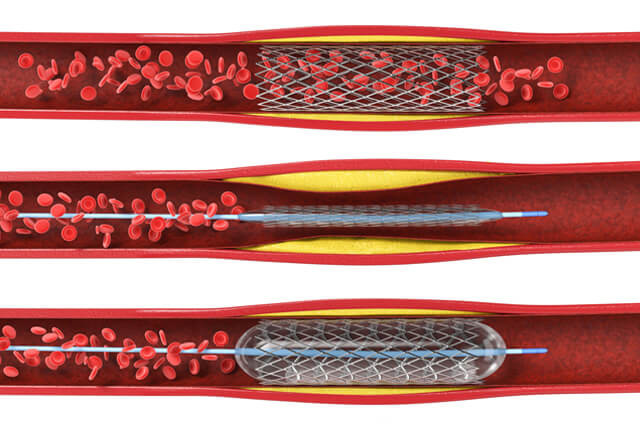
Coronary interventions (angioplasty, stents, thrombectomy, atherectomy)
For patients with narrowed or blocked coronary arteries, we offer procedures like angioplasty, stenting, and thrombectomy. These methods restore blood flow, prevent further damage, and improve heart function.
Peripheral angiography and interventions
Atherosclerosis can narrow arteries throughout the body, disrupting circulation. Peripheral angiography helps diagnose and treat issues in arteries like the aorta, renal arteries, and leg vessels.
Structural heart interventions
We provide minimally invasive treatments for structural heart conditions, such as valve degeneration or congenital defects. These advanced methods reduce recovery times and improve outcomes compared to traditional surgery.

Pacemaker implantation
We treat patients with slow heart rhythms by implanting pacemakers. These small devices help regulate and stabilize the heart’s electrical activity.

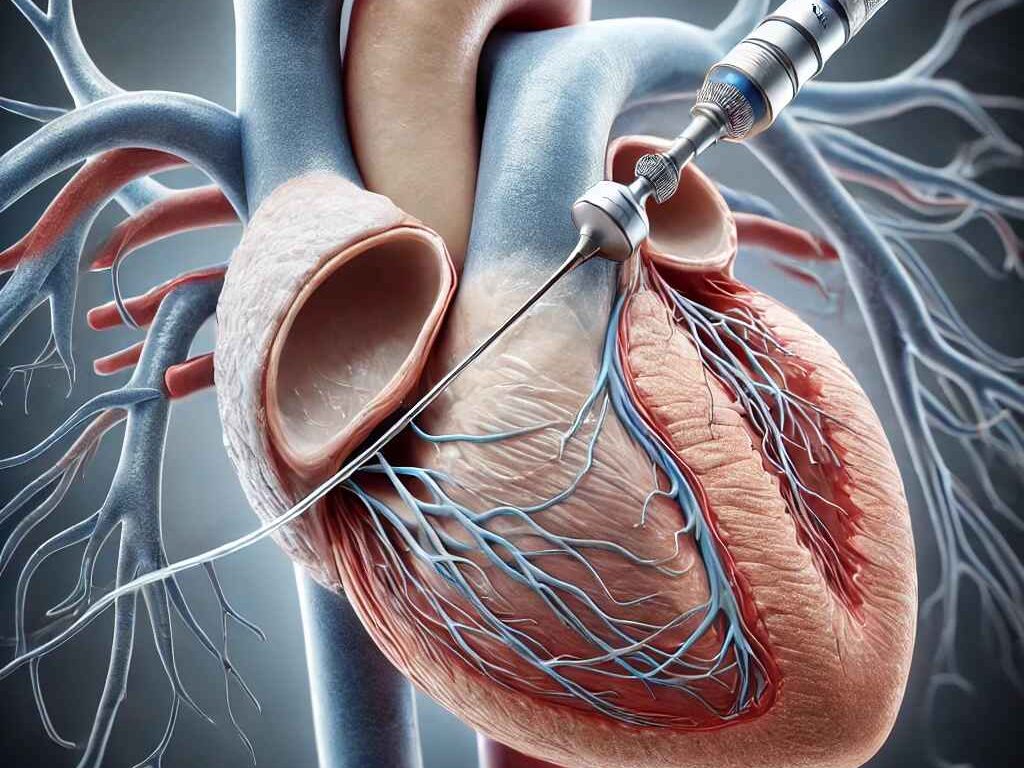
Transesophageal echocardiography
For detailed heart images, we perform transesophageal echocardiography (TEE). This procedure uses a specialized ultrasound probe inserted into the esophagus. Sedation ensures patient comfort during the process.
